There are 3 types of Thoracic Outlet Syndrome (TOS): Neurogenic, Arterial and Venous.
The anatomical boundaries associated with these syndromes are the same for Neurogenic and Arterial and completely different for Venous. This means that there are really 2 areas to consider in treatment of these problems and so I refer to only Neuroarterial and Venous.
Neuroarterial TOS
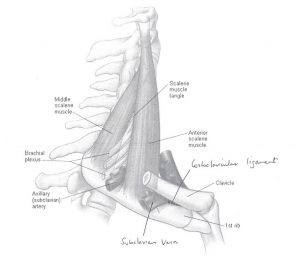
The brachial plexus and subclavian artery course through a triangle as they make their way to the arm. The triangle is bounded by scalenus anterior and scalenus medius at the front and back with the first rib as the base.
Nerve symptoms or arterial compression are caused by the space being reduced especially during elevation and external rotation of the arm, such as movements made when brushing your hair or when hanging washing on the clothesline.
If these symptoms become troublesome, the first step is physiotherapy by an experienced practitioner in this area. If exercises and strengthening programs fail after an extended trial of treatment, consideration may be given to decompression of the thoracic outlet by surgical means.
Neuroarterial TOS Operation & Recovery
The Operation
The operation is designed to remove the front wall and floor of the triangle described above to allow for much more room in this space so that there is no compression of either major structure when using the arm.
The incision is made just above the collarbone and usually measures about 7 centimetres. Of course, the length of an incision depends on the size of the patient and the access available. This means that there will be a scar in this region but it will fade over time.
There is a lot of anatomical traffic through this area, including the nerve to the diaphragm (phrenic nerve) and the lymphatic ducts, as well as the subclavian artery and brachial plexus of nerves that are going to be decompressed. All of these things are at risk during the procedure, so it is important to select a surgeon who is familiar with this territory in order to minimise the chances of adverse events. In experienced hands, the risks of intervention are quite small.
Other potential complications include bleeding and infection (as with all surgery) and pneumothorax and haemothorax which occur when some air or blood gets into the thoracic cavity around the lung. Very rarely would these collections need to be drained.
Recovery
Following surgery, the hospital stay is usually in the order of 2 to 3 nights. During this time you will be given exercises to do by the hospital physiotherapist, which should be continued at home.
Dr Campbell will usually see you again at 6 weeks post-op when you will have an ultrasound to confirm effective decompression.
Please note: that the resolution of symptoms is not usually immediate and there will be a period of about 6 months where there may still be symptoms that are present. These will gradually fade over time.
Cervical Rib TOS
This is a special case of TOS where a complete or partial extra rib coming from C7 (the lowermost neck vertebra), and usually arising within scalenus medius pushing the brachial plexus of nerves and the subclavian artery forward so that they are draped over the front of the rib and put on the stretch.
This arrangement can cause nerve symptoms and arterial degeneration to aneurysm formation resulting in possible embolisation from the aneurysm into the hand. This means clot particles can gradually obstruct the arteries in the arm and hand which can lead to a lack of blood supply and eventually possible gangrene of the fingers.
Cervical Rib TOS Treatment
The treatment of this condition is to remove the rib via an operation above the collarbone and fix the aneurysm if required to prevent further embolisation.
Dr Campbell has been performing excision 1st rib surgeries since 2011 and has performed 154 operations since that time.
Venous TOS
Venous TOS usually presents with a painful blue swollen arm due to thrombotic occlusion (blood clot blockage) of the subclavian vein. Veins along the affected arm will be distended and there may be new prominent veins developing across the chest wall, which are new collateral that are opening to bypass the blockage in the vein.
The subclavian vein drains blood from the arm to the chest via the superior vena cava into the heart. Just before it enters the chest, it passes through a triangle bounded by the clavicle and the muscle underneath it (subclavius muscle) at the top and the first rib below with the base of the triangle, being the scalenus anterior muscle as it attaches to the first rib. If this triangle is reduced in size, there will be compression of the vein during movement, which will cause repeated injury to the vein over time and eventually lead to blockage of the vein by clot formation.
Patients with this presentation are often young and athletic, and over time the muscles bordering the triangle described above have become larger, reducing the space significantly.
Venous TOS Treatment
The essence of treatment involves:
- Dissolving the clot as soon as possible using thrombolytics (clot dissolving medicine), delivered whilst doing the diagnostic venogram in the angiogram suite.
- As soon as possible, decompressing the triangle with removal of the inner part of the first rib with division of the scalenus anterior muscle and excision of the subclavius muscle, and division of ligaments at the apex of the triangle (costoclavicular ligaments).
- Fixing the vein if required. This may require opening the vein and putting in a patch to make the vein wider. The patch of vein is usually taken from the leg.
- Another venogram upon completion, with the possibility of needing a stent to maintain flow.
- Anticoagulation for 3 to 6 months.
The operative part is achieved through an incision about 7 to 10 centimetres long below the inner part of the collarbone. Another approach is an incision in the axilla (armpit), but having done this for many years with limitation of vein and access to the important structures, this method is no longer used.
If you would like to discuss your symptoms with Dr Campbell

